Your go-to resource for everything you need to know about living the dream in sunny Spain.
As an expat who has fallen in love with the Spanish lifestyle, I’m here to share my experiences, tips, and tricks to help you make the most out of your life in this beautiful country.
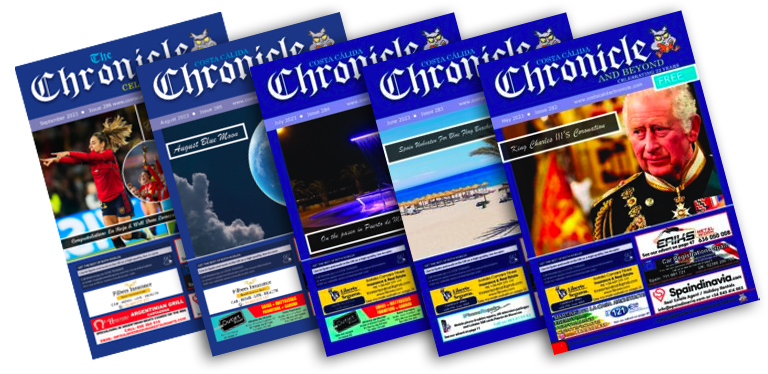
Want to read The Chronicle online? See the latest and previous copies here.